So, What Is A Retinal Tear Or Detachment?
This condition can impact vision significantly and requires prompt medical attention to prevent long-term damage.
What Causes Retinal Tears or Detachment?
Trauma: Physical injury to the eye may cause damage and lead to detachment.
Severe Nearsightedness (Myopia): Individuals with high myopia are at greater risk due to thinner retinas.
Previous Eye Surgery: Procedures such as cataract surgery may elevate risk levels.
Symptoms of a Retinal Tear or Detachment
It’s essential to recognize symptoms early.
Sudden appearance of floaters (small shadows or spots in vision)
Flashes of light in peripheral vision
A shadowy curtain effect over a portion of your visual field
Blurred or reduced central vision
These symptoms should not be ignored and warrant seeking care from an eye specialist.
Types of Retinal Conditions
Type | Description |
Retinal Tear | A small break in the retina that may lead to fluid leaking underneath it. |
Retinal Detachment | Occurs when fluid collects under the retina, causing it to lift away completely from its underlying layers. |
Both conditions require timely intervention but differ in severity. While retinal tears can often be treated before worsening, detachments usually require more involved surgical options.
Risk Factors
Aging adults (especially over age 50)
Individuals with extreme nearsightedness
Those who have experienced previous retinal issues
People with certain medical conditions like diabetes
History of prior trauma or eye injuries
Early detection and awareness play a critical role in preserving optimal vision outcomes when dealing with these conditions.
When it comes to addressing a retinal tear or detachment, a variety of medical procedures can help repair the damage and preserve vision.
Common Treatment Approaches
A freezing treatment applied directly to the retinal tear using a cryoprobe.
This method helps form scar tissue that stabilizes the retina.
A surgical procedure where vitreous gel (the clear substance in the eye) is removed and replaced with saline, gas, or silicone oil.
Effectively addresses more severe retinal detachments by relieving traction or pulling on the retina.
Factors Influencing Treatment Choice
Severity:Larger tears or full detachments may require surgical intervention (e. g. , vitrectomy or scleral buckle), while smaller tears may respond well to non-invasive options like laser photocoagulation.
Location:Tears near critical areas such as macula often require prompt attention with precise techniques.
Patient Health:Underlying conditions like diabetes or previous eye surgeries could affect treatment recommendations.
Post-Treatment Care
Follow all instructions provided by your healthcare provider regarding medications and activity restrictions.
Report any symptoms such as increased floaters, light flashes, or worsening vision immediately.
Attend follow-up appointments diligently for monitoring progress and ensuring long-term success.
Each patient’s condition is unique; therefore, consultation with an ophthalmologist is essential in determining which treatment would be most effective based on individual needs.
Vitrectomy
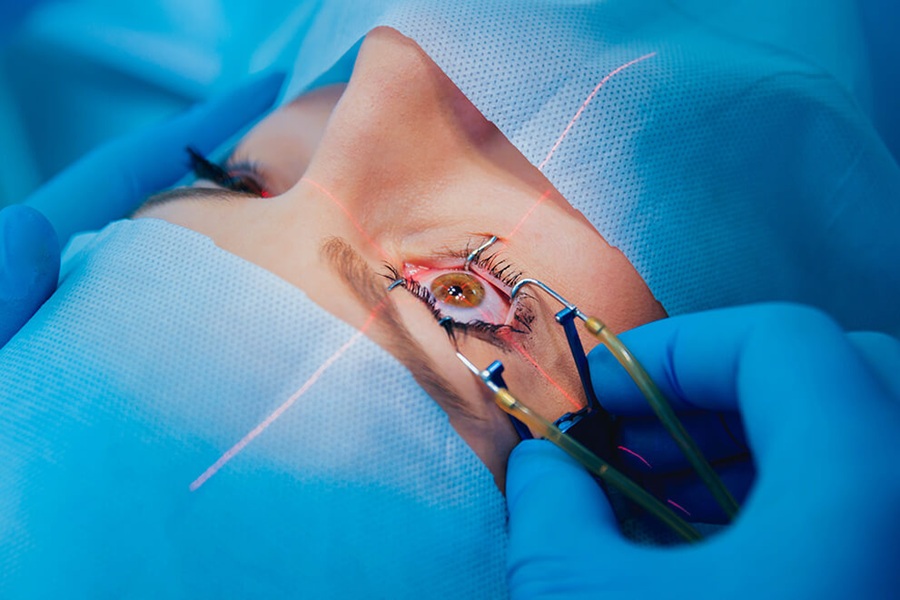
Vitrectomy is a surgical procedure often used to repair retinal tears or detachments. By removing this gel, surgeons can manipulate and reattach the retina more effectively.
Purpose of a Vitrectomy
A vitrectomy may be recommended for cases where:
- Retinal scar tissue (proliferative vitreoretinopathy) is present, pulling on the retina.
- Blood or debris in the vitreous (due to bleeding or infection) obstructs visibility.
This approach is frequently combined with other techniques to ensure proper reattachment and healing of the retina.
Steps Involved in a Vitrectomy
1.Anesthesia:2.Small Incisions:Tiny openings are made in the sclera (the white part of your eye). These allow surgical instruments to enter. 3.Removal of Vitreous Gel:4.Retina Repair:Depending on the issue, surgeons may reattach the retina using methods such as laser treatment or cryotherapy (freezing treatment).
5.Replacement Fluid:Over time, these substances are naturally replaced by fluid produced within your eye.
Recovery After a Vitrectomy
Activity Restrictions:Avoid heavy lifting or strenuous activities during recovery.
Follow-up Appointments:Regular check-ins with your specialist ensure proper healing and monitor vision improvement.
Potential Risks and Benefits
Benefits
- Restores vision by reattaching the retina properly.
- Addresses underlying complications that may worsen without treatment.
Risks
- Development of cataracts over time due to changes induced by surgery.
- Possible risk of infection or increased intraocular pressure.
By following medical recommendations pre-and post-surgery, patients can maximize their chances for optimal outcomes after undergoing vitrectomy procedures tailored specifically for retinal tears or detachments.
Scleral Buckle
Scleral buckle surgery is one of the established procedures to repair a retinal detachment.
How Does Scleral Buckle Work?
This adjustment allows the detached retina to come back into contact with the underlying tissue, promoting proper healing and restoration.
What Happens During the Procedure?
Anesthesia: Scleral buckle surgery is usually performed under local or general anesthesia.
PlacementThis band remains in place permanently unless removal becomes necessary for some reason later on.
Sealing Tears: Retinal tears are typically sealed at this time using cryotherapy (freezing treatment) or laser photocoagulation to ensure they do not reopen after surgery.
Recovery Process
After scleral buckle surgery, patients are usually given specific post-operative care instructions to promote healing and minimize complications, such as:
- Avoiding heavy lifting or strenuous activities for several weeks. - Using prescribed eye drops regularly to reduce inflammation. - Attending follow-up appointments for monitoring progress.
Some individuals may experience temporary side effects like redness, discomfort, or blurred vision while recovering from this procedure.
Advantages | Considerations |
High success rate | Possible side effects like double vision |
Suitable for various types of detachments | May require additional procedures |
Long-lasting solution | Minor changes in refractive error |
When Is Scleral Buckle Recommended?
This procedure is often used in cases where retinal tears are extensive or complex, particularly when other treatments like laser therapy alone may not suffice. It’s also a common choice when there are multiple tears causing traction that needs stabilization.
Scleral buckle has been widely utilized for decades due to its effectiveness and ability to preserve vision in many patients with retinal detachment concerns.
Pneumatic Retinopexy
It is often considered for retinal detachments that are relatively simple and do not involve extensive damage or tears located in difficult-to-reach areas.
How Does Pneumatic Retinopexy Work?
Repositioning: Once injected, this bubble rises to press against the detached portion of the retina, helping it reattach to the underlying tissue (the retinal pigment epithelium).
Sealing Tears: To secure the torn area of the retina, other techniques such as laser photocoagulation or cryopexy (freezing) may be applied during or after this procedure. These methods create scar tissue around the tears, ensuring they stay sealed and preventing further detachment.
When Is Pneumatic Retinopexy Recommended?
This technique is typically recommended in specific cases such as:
- Small or uncomplicated retinal detachments.
- Detachments where tears are located in the upper portion of the retina (as gas rises and works best in these positions).
- Patients who are unable to undergo more invasive surgical options due to health conditions or other contraindications.
Benefits of Pneumatic Retinopexy
- Minimally invasive
- Quicker recovery time compared to major surgeries like scleral buckle or vitrectomy.
- Preservation of eye structure since this method doesn’t involve removing parts of the vitreous humor.
Limitations and Considerations
Limitation/Consideration | Description |
Positioning Requirements | Patients must maintain specific head positions for several days following surgery so that the gas bubble stays in place over the damaged area. This requirement might be difficult for some individuals. |
Not Suitable for Complex Cases | Larger or more complex retinal detachments usually require alternative procedures like vitrectomy or scleral buckle. |
Temporary Vision Changes | Vision may remain blurry while the gas bubble is present; normal vision typically resumes after it dissipates over time (usually within weeks). |
Post-Procedure Care
Proper post-procedure care plays a critical role in achieving successful outcomes: - Maintain proper head positioning as instructed by your ophthalmologist. - Avoid air travel until cleared by your doctor, as changes in atmospheric pressure can cause complications with a gas-filled eye. - Attend all follow-up appointments to monitor healing progress.
Pneumatic retinopexy offers an effective solution for specific retinal detachment cases when performed under appropriate circumstances and with proper aftercare adherence.
Pneumatic Retinopexy
This technique is most suitable for uncomplicated retinal detachments where the tear is located in the upper portion of the retina and can be sealed effectively.
How It Works
Once positioned correctly, additional treatments such as laser photocoagulation or cryopexy are employed to seal the retinal tear and secure it permanently.
Step-by-Step Overview
After the procedure, patients are often instructed to maintain a specific head position for several days.
Laser or freezing treatments (cryotherapy) are applied to permanently seal any tears in the retina.
Advantages
Minimally invasive compared to some other surgical procedures like vitrectomy or scleral buckle.
Often less costly and shorter than more complex surgical alternatives.
Limitations
Not suitable for all types of retinal detachments, particularly those involving multiple tears or lower sections of the retina.
Requires strict adherence to head positioning instructions post-procedure for optimal results.
Criteria | Pneumatic Retinopexy |
Suitability | Upper retinal detachments; single or limited tears |
Setting | Outpatient |
Recovery Time | Relatively short |
Post-Procedural Care | Strict head positioning required |
Additional Treatment | Laser photocoagulation or cryotherapy needed |
Considerations
Patients undergoing pneumatic retinopexy should discuss their specific condition with their ophthalmologist to determine whether this method is appropriate for their case. Success rates are generally high when patients adhere to post-procedure instructions diligently. However, some cases may require additional interventions if complications arise or if complete reattachment is not achieved on initial treatment.
This procedure remains an effective option within modern ophthalmology for treating select cases of retinal detachment while minimizing surgical risks and recovery time compared to other methods.
Pneumatic Retinopexy
How Pneumatic Retinopexy Works
Positioning of the Patient: Following the injection, you may be asked to maintain a specific head position for several days to allow the gas bubble to float and press against the detached retina effectively.
Sealing Retinal Tears: After repositioning, laser photocoagulation or cryotherapy is often used to seal retinal tears or holes permanently. These techniques create a bond between the retina and its underlying supportive tissue.
Recovery Process
Recovery from pneumatic retinopexy involves adhering closely to post-procedure instructions provided by your healthcare provider, as proper positioning of your head plays a critical role in achieving success with this treatment.
Head Positioning: Patients are typically instructed to keep their head in a certain position (e. g. , face down) for several hours each day over one or more weeks so that gravity can help hold the retina in place while it heals.
Activity Restrictions: You may need to avoid activities like air travel until your doctor confirms that it’s safe since changes in altitude can affect gas pressure within your eye.
Visual Changes: Vision may be temporarily blurry due to the presence of the gas bubble; as it gradually absorbs over time (usually weeks), normal vision should begin returning.
Aspect | Detail |
Procedure Type | Minimally invasive |
Gas Used | Sulfur hexafluoride or perfluoropropane |
Success Factors | Head positioning and adherence to recovery protocol |
Common Risks | Possible increased pressure in eye, recurrence risk |
Possible Risks and Considerations
As with any medical intervention, pneumatic retinopexy has potential risks such as elevated intraocular pressure, cataract formation, or recurrence of retinal detachment. It’s essential for patients undergoing this procedure to have close follow-up care with their ophthalmologist.
Pneumatic retinopexy has proven effective for many cases when performed under appropriate conditions, making it an important treatment option for addressing retinal detachments without requiring extensive surgery like scleral buckling or vitrectomy. Proper evaluation by an ophthalmologist will determine whether this method is suitable based on individual circumstances.









